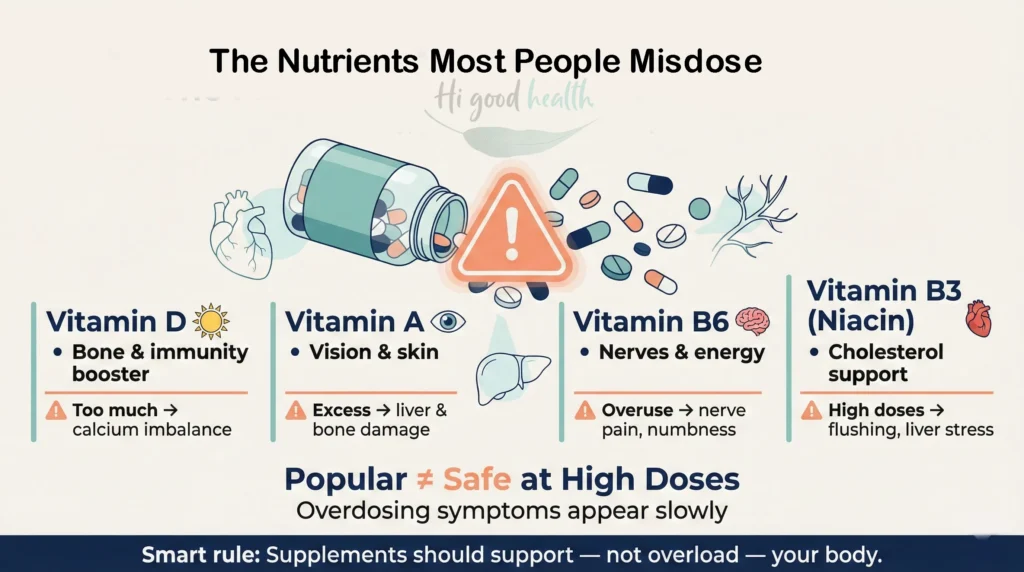
We all know vitamins are good for us, but did you know some of them are often taken in the wrong amounts? Vitamins like D, A, B6, and B3 (niacin) are some of the most commonly misdosed.
You may ask why? Because they’re popular, widely recommended, and often misunderstood. Many people take extra doses of vitamins through supplements, hoping for better energy, stronger immunity, or glowing skin, without realising that too much of a good thing can actually be harmful.
The tricky part? Symptoms of vitamin overdose usually creep in slowly. So, it’s important to know which vitamins are most often misdosed and why. Let us read on to know more.
What Are the Most Commonly Misdosed Vitamins?
Not all vitamins are misdosed equally; some are far more likely to be taken in the wrong amounts, either too much or too little. The issue is that most people do not even realise they are overdoing it. Let’s take a look.
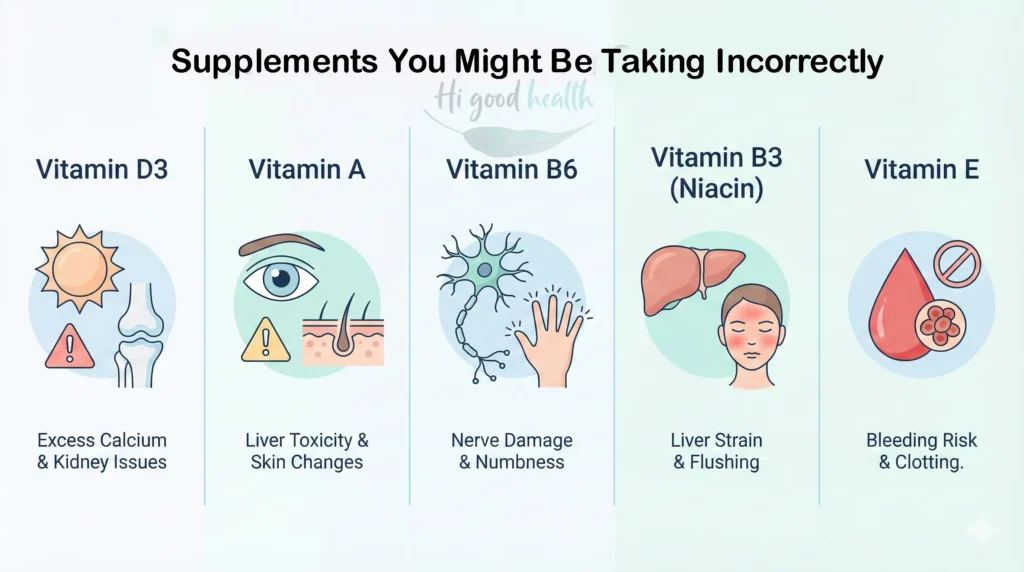
- Vitamin D3: A popular choice for bone health and immunity. But too much can raise calcium levels in the blood, leading to nausea, kidney issues, and even organ damage over time.
To know more about protecting your kidneys from supplement harm, check our detailed blog
- Vitamin A: Often found in skin and eye supplements. It builds up in the body easily and can cause headaches, liver problems, and blurred vision when taken in excess.
- Vitamin B6: Known for supporting mood and energy. Long-term high doses can lead to nerve damage and a tingling sensation in the hands and feet.
- Vitamin B3 (Niacin): Used to manage cholesterol. But in high amounts, it may cause liver damage, skin flushing, and even digestive upset.
- Vitamin E: Taken for its antioxidant benefits. Overdoing it may interfere with blood clotting and, in rare cases, increase the risk of stroke.
These vitamins are essential, but they’re also the ones that are easiest to misdose. The key takeaway? More isn’t always better, especially when it comes to fat-soluble vitamins that stay in your system longer.
Read more: https://www.ncbi.nlm.nih.gov/books/NBK538510/
Water-Soluble vs. Fat-Soluble: Why It Matters
Vitamins come in two main types, water-soluble and fat-soluble, and this makes a big difference in how your body handles them.
Water-soluble vitamins like vitamin C and the B-complex group dissolve in water and leave your body through urine. So even if you take a bit more, your body usually flushes it out.
Fat-soluble vitamins like A, D, E, and K, on the other hand, get stored in your fat tissues and liver. That means if you keep taking too much, they can build up and cause toxicity or long-term health issues. That’s why fat-soluble ones need extra care.
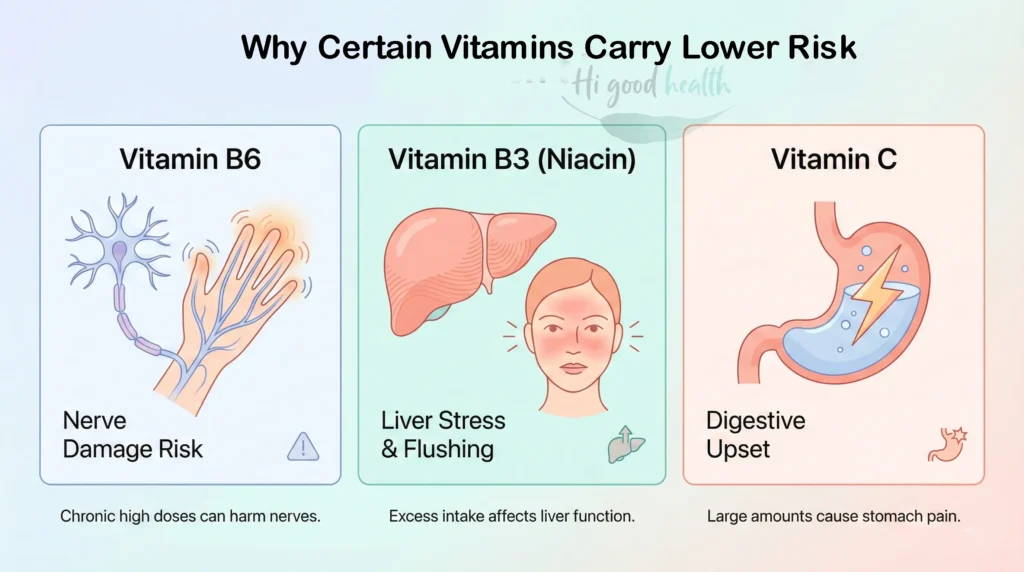
Why Water-Soluble Vitamins Are Safer (But Not Risk-Free)
Although the water soluble vitamins are excreted through urine however this doesn’t mean that they are completely risky. For instance, high doses of vitamin B6 (pyridoxine) over prolonged periods have been linked to sensory neuropathy, causing symptoms such as numbness, tingling, and difficulty walking.
Similarly, niacin (vitamin B3) at doses above 1–3 grams per day can lead to liver toxicity and severe flushing, sometimes accompanied by nausea and abdominal pain.
Even vitamin C, often seen as harmless, can cause gastrointestinal disturbances like diarrhoea, cramps, and nausea when taken in doses over 2,000 mg per day. In rare cases, extremely high doses may trigger migraines.
So, while the body’s ability to flush out excess water-soluble vitamins generally protects you, consistently exceeding recommended intakes can lead to serious health issues. It’s important to respect dosing guidelines even for these “safer” vitamins.
Fat-Soluble Vitamins: Small Overdose, Big Trouble
Unlike water-soluble vitamins that flush out quickly, even a small overdose of fat-soluble vitamins can cause serious health problems.
Vitamin A overdose can lead to symptoms like headaches, nausea, dizziness, and in severe cases, liver damage, bone pain, and increased pressure inside the skull. Too much Vitamin A during pregnancy causes birth defects.
Vitamin D overdose causes high calcium levels in the blood, which can result in nausea, weakness, kidney damage, and irregular heartbeats.
Vitamin E in excess can interfere with blood clotting, raising the chance of bleeding problems and stroke, especially if you’re on blood thinners.
Because these vitamins accumulate, it’s important not to exceed recommended doses. Even small extra amounts taken regularly can lead to big trouble for your organs and overall health.
Read More: https://en.m.wikipedia.org/wiki/Vitamin_D_toxicity
Checkout the Verified Normal Blood Test Reference Ranges:
| Vitamin | Typical Reference Range | Units | Notes |
| Vitamin D3 (25(OH)D) | 20 – 50 (sometimes 30 – 100) | ng/mL | Levels <20 ng/mL usually indicate deficiency; some labs set sufficiency at >30 ng/mL. |
| Vitamin A | 20 – 60 | mcg/dL | Serum retinol levels; some labs report in μmol/L (0.7–2.2 μmol/L). |
| Vitamin B6 | 5 – 50 | ng/mL | Measured as pyridoxal 5′-phosphate (PLP), the active form of B6. |
| Vitamin E | 5.5 – 17 | mg/L | Typically measured as alpha-tocopherol. |
| Vitamin B12 | 200 – 900 | pg/mL | Levels <200 pg/mL generally suggest deficiency. |
Important Notes:
- Vitamin D: Some labs consider >30 ng/mL as optimal; below 20 ng/mL is usually deficient.
- Vitamin A: Units can vary (mcg/dL or μmol/L), so be sure to match your lab’s units.
- Vitamin B6: The active form (PLP) is typically tested.
- Vitamin E: Labs measure alpha-tocopherol; values can vary by lab and population.
- Vitamin B12: Deficiency generally below 200 pg/mL.
How to Know How Much Vitamin You Really Need
Not everyone needs the same amount of vitamins. Your ideal dose depends on your age, diet, medical conditions, and whether you actually have a deficiency.
Taking random supplements based on what the label says or what others are taking can do more harm than good. The safest way to find out what your body needs is by getting tested. Here’s a simple guide to which blood tests help identify specific vitamin and mineral deficiencies.
To learn more about supplement guidance for seniors, read our in-depth blog
| Nutrient | Blood Test | Deficiency Signs |
| Vitamin D | 25(OH)D (25-hydroxyvitamin D) | Weak bones, fatigue, and low immunity |
| Vitamin B12 | Serum B12 | Tingling hands/feet, memory issues |
| Iron | Ferritin, Iron, TIBC | Fatigue, pale skin, short breath |
| Folate (B9) | Serum folate | Mouth sores, poor concentration |
| Magnesium | Serum magnesium | Muscle cramps, irregular heartbeat |
| Calcium | Serum calcium | Muscle spasms, brittle nails |
| Zinc | Plasma zinc | Hair loss, slow wound healing |
| Omega-3 | Omega-3 Index or RBC EPA/DHA | Dry skin, brain fog, joint pain |
| Iodine | Urinary iodine concentration | Thyroid issues, weight gain |
Read more: https://www.betterhealth.vic.gov.au/health/healthyliving/vitamin-and-mineral-supplements
How to Avoid Vitamin Misdosing in Daily Life
Vitamin overdosing is more common than people think—and it often happens unintentionally. To stay safe and get the full benefit of your supplements, here are a few medically sound tips:
1. Always Consult Your Doctor
Before starting any supplement, speak to a healthcare professional. Your doctor may recommend blood tests to assess actual needs and avoid unnecessary intake.
2. Avoid Megadoses Unless Prescribed
More is not always better. High doses of fat-soluble vitamins (A, D, E, K) can build up in the body and cause toxicity.
3. Track Your Supplement Intake
Keep a log of all vitamins, multivitamins, and herbal products you take. Overlapping ingredients can quietly lead to overdosing.
4. Check for Fortified Foods
Many cereals, juices, and snacks are fortified with extra vitamins. If you’re taking supplements on top of that, you might exceed safe limits.
5. Read Labels Carefully
Watch for the % Daily Value (%DV). Anything over 100% should raise a red flag unless medically required.
6. Reassess Regularly
Your needs change with age, health conditions, diet, and lifestyle. What you needed a year ago may not be necessary today.
Key takeaway
Your best approach is a personalized one. Do not rely on general recommendations or online trends. Testing, tracking, and tailoring your supplement use is key to safe and effective nutrition.
FAQs
Yes. While vitamins are essential, “too much of a good thing can actually be harmful”. High doses, especially of fat-soluble vitamins, can accumulate in the body and cause toxicity, organ damage, or long-term health issues.
Fat-soluble vitamins like A, D, E, and K are the riskiest because they are stored in fat tissues. However, water-soluble vitamins like B6 and Niacin can also cause nerve or liver damage if taken in high doses.
Symptoms often “creep in slowly” and can include nausea, headaches, weakness, and digestive upset. High doses of Vitamin B6 specifically can lead to a tingling sensation or numbness in the hands and feet.
Not necessarily. While the body flushes excess water-soluble vitamins, high doses are not risk-free. Vitamin C over 2,000 mg can cause cramps and nausea, while long-term high B6 intake is linked to nerve damage.
out what your body needs is by getting tested” rather than guessing. Blood tests like 25(OH)D for Vitamin D can confirm actual deficiencies, preventing you from taking “random supplements” unnecessarily.
Can I take supplements if I eat fortified foods?
Be cautious. Many cereals, juices, and snacks are fortified with extra vitamins. If you combine these with supplements, you might unknowingly exceed safe limits, so it is vital to read labels carefully.
Not everyone needs the same amount. Your ideal dose depends on your “age, diet, medical conditions,” and deficiency status. Consult a doctor to tailor your intake rather than relying on general trends or “random supplements”.
