Humans have always sensed a connection between the gut and the brain—whether it is a “gut feeling,” a “gut-wrenching” experience, or a sudden bowel movement during moments of stress. But until recently, science had no clear explanation for this.
Now, research is uncovering just how powerful this link truly is. Your digestive system is not just responsible for breaking down food but it also plays a key role in how you feel, think, and behave.
In fact, your gut has its own neural network, known as the “second brain.” This system constantly sends signals to your brain. It shapes your mood, decision-making, and emotional responses. So, understanding this communication pathway could transform the way we view mental health and overall well-being. Let’s read on to know more
What Is the Gut-Brain Axis, and Why Does It Matter?
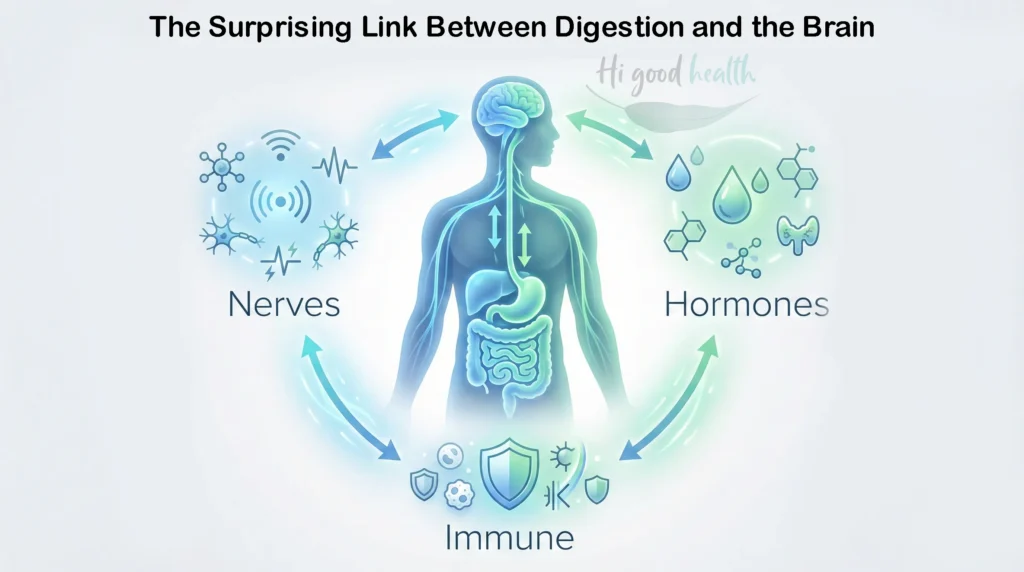
The gut-brain axis is a two-way communication system between the gastrointestinal tract and the central nervous system. It involves neural pathways, especially the vagus nerve, as well as hormones and immune signals. This system allows your gut and brain to exchange information in real-time.
When your gut is in balance, this system supports calmness, clarity, and emotional control. But when it’s out of balance, it can contribute to anxiety, depression, and even memory issues.
Read more: Learn from Frontiers in Psychiatry
- Information flows both ways—from the brain to the gut and back.
- The vagus nerve acts as a primary channel for this communication.
- Hormones and immune signals play a supportive role in signal exchange.
- Disruption in this system can impact both digestion and mental clarity.
Restoring balance may improve both mood and gut function.
How Do Hormones and Immune Signals Influence the Gut-Brain Axis?
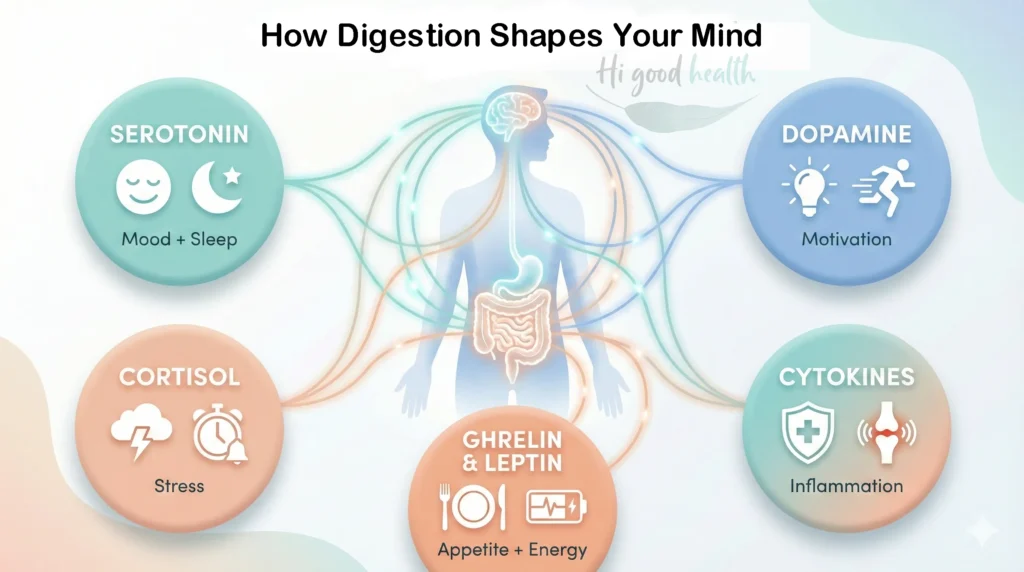
Several key messengers help the gut and brain communicate effectively. These include hormones and immune molecules that impact your mood, stress levels, and overall mental health.
1. Serotonin
- About 90% of serotonin is produced in the gut.
- It helps regulate mood, sleep, and digestion.
- An imbalance can lead to anxiety or depression.
2. Dopamine
- Also produced in the gut in smaller amounts.
- Affects motivation, pleasure, and reward.
- Low levels are linked to mood disorders.
3. Cortisol
- Known as the stress hormone.
- Released by the adrenal glands but influenced by gut health.
- Chronic gut inflammation can raise cortisol levels, increasing stress and anxiety.
4. Cytokines (immune signals)
- These are proteins released during immune responses.
- High levels from gut inflammation can interfere with brain function.
- Linked to brain fog, fatigue, and depressive symptoms.
5. Gut peptides : Ghrelin & Leptin
- Influence appetite and also impact emotional behavior.
- They can signal the brain about hunger and fullness, affecting mood and energy levels.
How Do Gut Microbes Communicate With the Brain?
Your gut contains trillions of microorganisms, collectively known as the microbiota. These microbes do more than aid digestion. They help produce neurotransmitters such as serotonin, dopamine, and GABA—chemicals that regulate mood and behavior.
About 90% of the body’s serotonin, often called the “feel-good” hormone, is made in the gut. When gut bacteria are diverse and balanced, they contribute to emotional resilience. But an imbalance—called dysbiosis—can disrupt this harmony. This disruption may lead to increased stress, mood swings, and a lower threshold for anxiety. If you want to learn more about choosing between enzymes and probiotics, read our blog
Can Digestive Problems Affect Emotional Well-Being?
Many individuals with gastrointestinal disorders—like irritable bowel syndrome (IBS), acid reflux, or constipation, often experience mental health symptoms. These include irritability, low energy, and feelings of nervousness.
It is not just psychological. The inflammation or discomfort in the gut sends distress signals to the brain. These messages can elevate cortisol levels, your body’s primary stress hormone. Elevated cortisol, in turn, intensifies both digestive and mental symptoms.
According to Harvard Health, the brain and gut are so closely connected that your digestive health can impact your emotional state significantly.
Read more: Explore Harvard’s full article here
- Gut disorders often coincide with mental fatigue or low motivation.
- Inflammation in the gut activates stress pathways in the brain.
- Elevated cortisol may worsen digestive discomfort.
- Recurrent gut issues can lead to persistent anxiety or irritability.
- Treating gut symptoms may help reduce emotional strain.
What Role Does the Vagus Nerve Play in Mental Health?
The vagus nerve acts as the main communication highway between the brain and the gut. It carries information both ways—sending brain instructions to the digestive system and vice versa.
Stimulation of the vagus nerve, either through deep breathing, meditation, or even certain probiotics, has been shown to improve mood and reduce symptoms of depression. Researchers are even exploring vagus nerve stimulation (VNS) as a therapeutic intervention for treatment-resistant depression.
How Can You Support the Vagus Nerve and Restore Gut-Brain Balance?
Restoring balance in the gut-brain axis can improve both mood and digestive health. The good news is, you can take simple, everyday steps to support the vagus nerve and enhance this powerful connection.
Try these proven lifestyle tips:
- Practice deep breathing
Slow, diaphragmatic breathing activates the vagus nerve and reduces stress hormones like cortisol. - Eat a gut-friendly diet
Include fermented foods (like yogurt, kefir, and kimchi) and high-fiber foods (like oats, legumes, and vegetables) to nourish gut bacteria. - Meditate regularly
Mindfulness and meditation calm the nervous system and enhance vagal tone. - Exercise consistently
Moderate physical activity, such as walking or yoga, supports both gut health and mental well-being. - Get enough sleep
Quality sleep helps regulate mood and supports the immune signals involved in gut-brain communication. - Stay socially connected
Positive social interactions have been shown to stimulate the vagus nerve and reduce symptoms of depression. - Try probiotics
Certain strains like Lactobacillus rhamnosus may support mood through their effects on the vagus nerve.
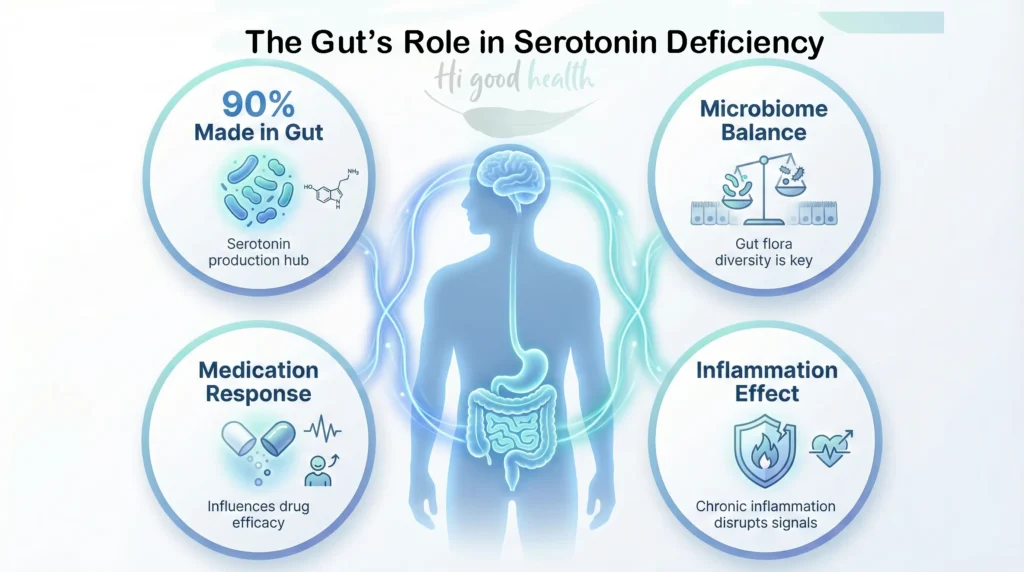
Is There a Gut Connection in Serotonin Deficiency Cases That Require Medication?
Yes, the gut still plays a significant role, even when someone has an inherent serotonin deficiency and needs medication like SSRIs (selective serotonin reuptake inhibitors).
Here’s how the gut may be involved:
- Majority of Serotonin Is Made in the Gut
Around 90% of the body’s serotonin is produced in the gut, not the brain. While brain serotonin directly affects mood, gut health influences how serotonin is made, stored, and signaled. - Gut Bacteria Impact Serotonin Levels
Certain gut microbes help produce or regulate serotonin. An imbalance in gut bacteria (dysbiosis) reduces serotonin availability and worsen mood issues. - Medication Effectiveness May Depend on Gut Health
Emerging research suggests that a healthy gut can enhance how well antidepressants work. Poor gut health might reduce the effectiveness of these medications or increase side effects. - Inflammation and Serotonin Disruption
Chronic gut inflammation can interfere with serotonin pathways, contributing to long-term mood disorders, even when medication is used. - Diet and Probiotics as Supportive Measures
While medication is crucial, supporting gut health with a balanced diet, probiotics, and anti-inflammatory foods may boost serotonin-related pathways and improve outcomes.
How Does Stress Impact Gut Health?
Stress triggers a gamut of chemical reactions in the body. These changes affect gut function almost instantly. You may notice bloating, cramps, or an upset stomach during stressful times. This is a biological response.
Chronic stress can increase gut permeability, allowing harmful substances to pass into the bloodstream. This can cause inflammation, which further disrupts the gut-brain balance. Over time, this cycle can contribute to both digestive disorders and mood disturbances.
- Stress can reduce blood flow to the digestive tract.
- It may increase stomach acid and irritate the intestinal lining.
- Gut bacteria composition can shift under prolonged stress.
- Chronic stress can weaken the intestinal barrier.
- Addressing stress is essential for long-term gut healing.
Can Probiotics Improve Mental Health?
Probiotics are live bacteria that support gut health. Certain strains have shown promising effects in improving mood and reducing anxiety. These are sometimes called “psychobiotics.”
Studies suggest that regular intake of specific probiotics can lower cortisol levels and increase serotonin production. However, not all probiotics are the same. Their effectiveness depends on the strain and individual health conditions.
- Lactobacillus and Bifidobacterium strains are often linked to improved mood.
- Probiotics can reduce inflammatory markers in the gut.
- They may enhance serotonin and GABA production.
- Clinical trials show reduced anxiety with daily probiotic intake.
- Consult a doctor before starting psychobiotic supplements.
What Foods Can Support the Gut-Brain Connection?
Your gut thrives on fiber-rich and fermented foods. Think whole grains, fruits, vegetables, yogurt, and kimchi. These foods feed your beneficial bacteria and reduce inflammation. On the other hand, processed foods, artificial sweeteners, and high sugar intake can harm your microbiome.
Including omega-3 fatty acids, found in flaxseeds, can also support brain health. Hydration, regular meals, and mindful eating further support digestive and emotional balance.
- Fiber supports healthy bacteria and improves bowel function.
- Fermented foods introduce beneficial bacteria into the gut.
- Omega-3s support both brain structure and gut integrity.
- Excess sugar may promote inflammation and bad gut bacteria.
- Balanced meals reduce fluctuations in mood and energy.
Is There a Link Between Gut Inflammation and Depression?
Yes, inflammation in the gut often leads to systemic inflammation, which has been strongly linked to depressive symptoms. Inflammatory cytokines can alter brain function and reduce the production of mood-enhancing neurotransmitters.
A poor diet, lack of sleep, and prolonged stress can all contribute to this cycle. Anti-inflammatory diets and proper gut care can be key strategies to restore mental balance.
Should Mental Health Treatment Include Gut Care?
A solid yes ! And science increasingly supports it. Mental health care is evolving beyond the traditional brain-only model, with integrative approaches now focusing on the gut as a key player in emotional and cognitive health. This shift is based on a growing body of research showing how the gut microbiome, inflammation, and digestion directly affect mood, behavior, and even psychiatric conditions.
Here’s how gut care fits into mental health treatment:
1. The Microbiome-Mood Connection
- Studies have found that people with depression and anxiety often have different gut bacteria profiles compared to healthy individuals.
- Specific strains like Lactobacillus and Bifidobacterium have shown promise in reducing anxiety and depressive symptoms in both animal and human trials. These are sometimes called “psychobiotics.”
2. Gut Inflammation and Brain Health
- Chronic low-grade gut inflammation can lead to the release of inflammatory cytokines, which cross the blood-brain barrier and affect neurotransmitter activity.
- This inflammatory process is increasingly linked to conditions like major depressive disorder and bipolar disorder.
3. Nutritional Psychiatry
- A diet rich in fiber, polyphenols, omega-3 fatty acids, and fermented foods supports a healthy gut environment and boosts the production of mood-regulating chemicals like serotonin and dopamine.
- The Mediterranean diet, for example, has been associated with lower risk of depression in numerous clinical studies.
To know more about recognizing early signs of cognitive decline, check out our in-depth blog
4. Personalized Gut Testing
- Emerging diagnostic tools such as 16S rRNA gene sequencing and whole-genome shotgun metagenomics now allow clinicians and researchers to analyze an individual’s gut microbiota with remarkable precision
- This opens the door to individualized treatment plans that combine conventional therapies with dietary changes, targeted probiotics, and supplements that are tailor made to the patient’s gut profile.
5. Complementary Therapies
- Practices like yoga, mindfulness, and deep-breathing exercises do more than reduce stress, they also stimulate the vagus nerve, enhancing gut-brain communication and regulating inflammation.
Importantly, gut-focused care doesn’t replace medications or therapy, especially for moderate to severe mental illness. But it offers a valuable, evidence-based layer of support that can improve the overall quality of life. For many patients, combining psychotherapy, medication, and gut health strategies creates a more holistic path to healing.
Why Should You Care About Your Gut-Brain Health?
Your gut and brain are in constant dialogue. What affects one often affects the other. Ignoring this relationship can delay healing, both mentally and physically. But nurturing your gut through good food, reduced stress, and probiotics can create a healthier, more balanced mind.
As research evolves, it is becoming clear that good mental health starts with good gut health. Start paying attention to your digestive system, it may be the key to how you feel, think, and live.
If you prefer a more visual version, check out our YouTube video here:
FAQs
Your gut is often called the “second brain” because it has its own neural network that sends constant signals to your brain. When your gut bacteria are balanced, this system supports calmness and emotional control. However, an imbalance can lead to mood swings, anxiety, and depression.
Common signs include irritability, low energy, and feelings of nervousness. Gut issues can also cause “brain fog,” fatigue, and depressive symptoms because inflammation in the digestive tract sends distress signals to the brain.
Stress triggers immediate chemical reactions that affect your gut function. It can increase stomach acid, reduce blood flow to the digestive tract, and cause cramps or bloating. Chronic stress also raises cortisol levels, which can intensify digestive discomfort.
Yes, certain probiotics, sometimes called “psychobiotics,” may help improve mood and reduce anxiety. Strains like Lactobacillus and Bifidobacterium are linked to improved mood because they can help lower cortisol (stress hormones) and increase serotonin production.
Remarkably, yes. About 90% of your body’s serotonin—the “feel-good” hormone that regulates mood and sleep—is produced in your gut. Your gut microbes play a key role in producing this essential chemical.
Focus on fiber-rich and fermented foods like yogurt, kefir, kimchi, whole grains, and vegetables. These foods feed beneficial bacteria and reduce inflammation. Omega-3 fatty acids found in foods like flaxseeds also support brain health.
No. Gut-focused care is a supportive strategy and does not replace medication or therapy for mental illness. However, supporting your gut with a healthy diet and probiotics may help medications work more effectively and reduce side effects.
You can stimulate the vagus nerve—the main highway between your gut and brain—through deep, slow belly breathing. This simple habit activates the nerve and reduces stress hormones. Meditation and social connection are also effective.
It can. High sugar intake and processed foods can harm your microbiome and promote bad bacteria. This often causes inflammation in the gut, which is strongly linked to depressive symptoms and can interfere with brain function.
To learn more about on how sweeteners affect your gut microbiome, read our detailed blog
