The boom nobody saw coming
GLP-1 weight-loss drugs didn’t just grow in popularity — they exploded into mainstream health care conversation. Recent U.S. survey data suggest that nearly 18 % of American adults say they have taken a GLP-1 drug at some point according to recent survey data, reflecting how widespread use has become beyond traditional diabetes care.
At the same time, telehealth and direct-to-consumer platforms have become major access points for these medications, with companies like Hims & Hers, Ro, LifeMD, PlushCare, and others incorporating GLP-1 consultations and prescriptions into their services — often making access feel faster and more convenient than traditional routes. https://www.hims.com/blog/hims-weight-loss-vs-ro
Pricing and delivery models vary significantly across providers, and patients are increasingly comparing options online as demand continues to grow.
But here’s the part that increasingly worries clinicians:
This boom is moving faster than patient education, long-term safety planning, and regulation can keep up.
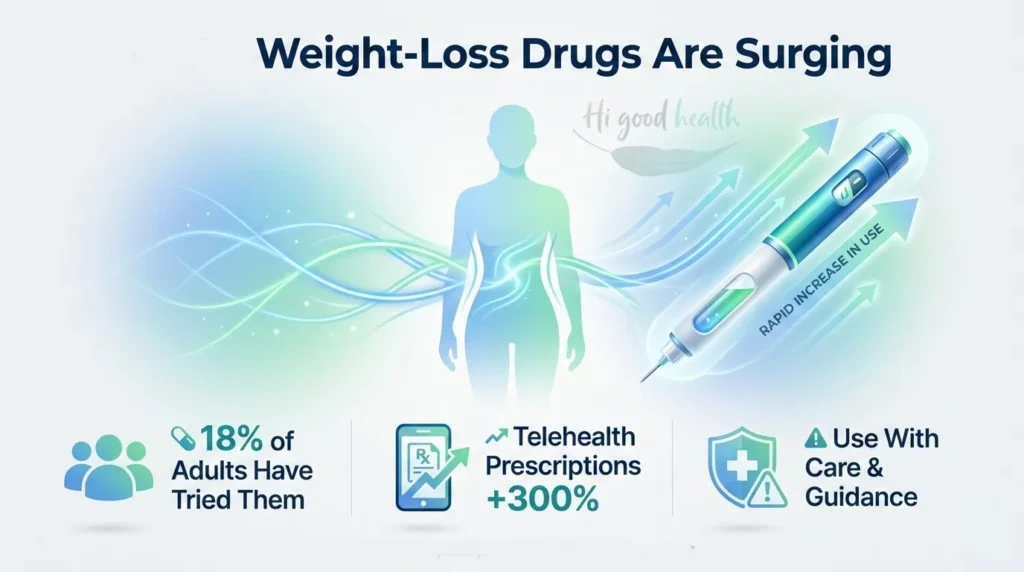
GLP-1 drugs can be transformative — but only when used with care, context, and continuity.
How GLP-1s evolved: from diabetes therapy to metabolic medicine
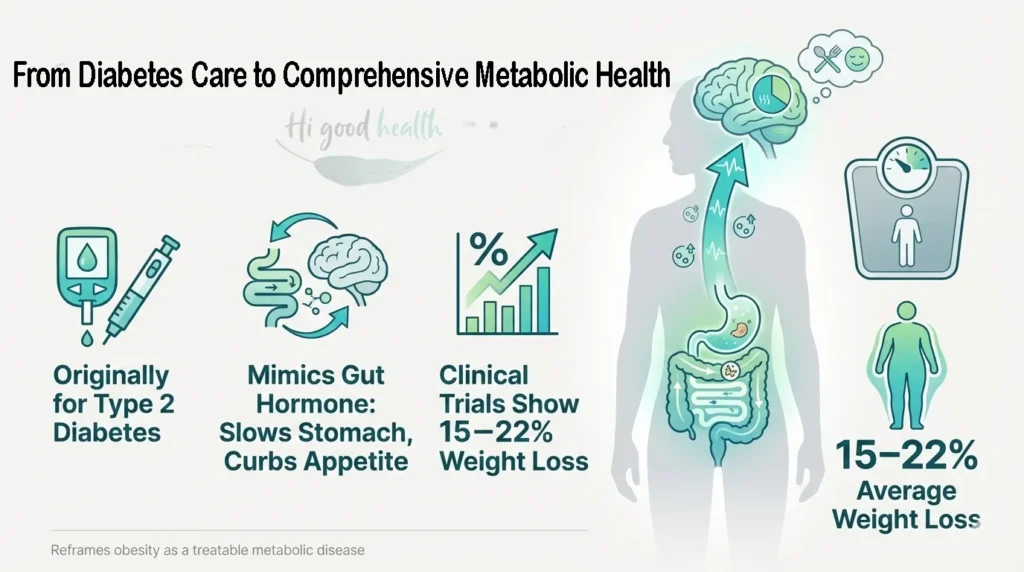
GLP-1 receptor agonists were originally developed to treat type 2 diabetes, not obesity. Researchers discovered that these medications mimic a naturally occurring gut hormone that enhances glucose-dependent insulin release, slows gastric emptying, and reduces appetite signals in the brain.
As large clinical trials progressed, consistent and clinically meaningful weight loss emerged as a secondary effect. When multiple studies demonstrated double-digit weight reduction, it became clear that these drugs had implications far beyond blood sugar control.
Between 2021 and 2023, landmark trials published in The New England Journal of Medicine and JAMA reported average weight loss ranging from approximately 15% to over 20%, significantly outperforming older weight-loss medications. Semaglutide demonstrated similarly meaningful reductions in people with obesityco. https://pubmed.ncbi.nlm.nih.gov/35658024/
This body of evidence helped reframe obesity as a chronic, treatable metabolic disease rather than a failure of willpower — marking a pivotal shift in modern medical thinking.
Why telehealth GLP-1 programs took off so fast
Telehealth didn’t rise because people wanted shortcuts. It rose because traditional healthcare systems failed to meet demand.
Many patients faced long wait times, insurance denials, or a lack of obesity-focused care. Telehealth filled that gap.
The real advantages
- Faster access in areas with few obesity specialists
- Lower upfront costs for uninsured patients
- Reduced stigma around seeking weight-loss care
- Convenience for people managing work, caregiving, or mobility limits
For many patients, telehealth provided their first serious medical conversation about weight.
That matters.
To know more about which diagnostic tests are really necessary, check out our in-depth blog
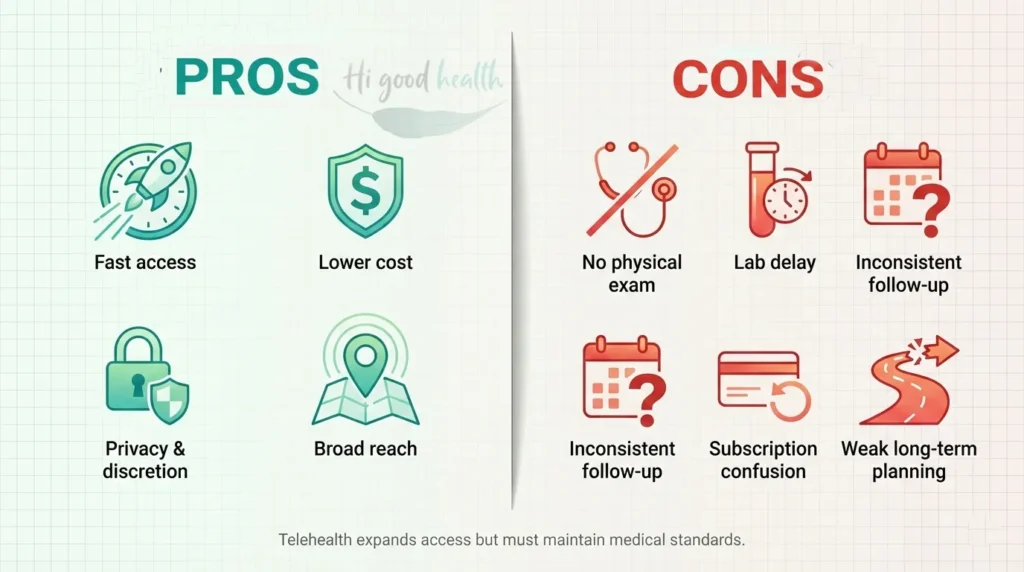
GLP-1 telehealth: the real pros vs cons
Pros
- Faster access than traditional clinics
- Lower initial cost
- Privacy and discretion
- Broader geographic reach
Cons
- No physical examination
- Labs often skipped or delayed
- Inconsistent follow-up
- Subscription billing confusion
- Weak long-term planning for stopping medication
Bottom line: Telehealth can expand access — but it must not dilute medical standards.
Top GLP-1 telehealth platforms in the U.S. (snapshot comparison)
| Platform | Typical Cost Range | FDA-Approved Options | Coaching Support | Notes |
| Ro | $$$ | Yes | Limited | Strong branding, higher cost |
| PlushCare | $$ | Yes | Minimal | PCP-style visits |
| LifeMD | $ | Mixed | Limited | Budget-friendly |
| Sequence (WW) | $$$ | Yes | Strong | Best lifestyle integration |
| Hims & Hers | $$ | Mixed | Limited | Heavy marketing focus |
Listings are illustrative, not endorsements. Availability, pricing, and prescribing practices change frequently – always verify directly.
Telehealth vs in-person care: which route makes sense?
Many patients face a practical decision:
Should I use telehealth—or pursue GLP-1 therapy through my local doctor and insurance?
In general:
- Telehealth may make sense if:
- Insurance coverage is denied or delayed
- Access to obesity specialists is limited
- You need faster initiation and are willing to self-advocate on monitoring
- In-person care may be preferable if:
- Your insurance covers FDA-approved GLP-1s
- You have complex medical conditions requiring hands-on evaluation
- You want integrated care with labs, imaging, and physical exams
Some patients use a hybrid approach—initiating therapy via telehealth while coordinating labs and long-term planning with their primary care physician. The key factor is not the platform, but continuity and medical oversight.
FDA-approved vs compounded GLP-1s: not the same, not “generic”
This distinction is widely misunderstood.
FDA-approved GLP-1 medications
Examples include Wegovy, Ozempic, Zepbound, and Mounjaro.
Important points:
- There is no FDA-approved generic semaglutide
- These drugs are patent-protected
- Delivered via pre-filled pens
- Standardized dosing
- Backed by large safety datasets
Compounded GLP-1 medications
Compounded drugs are custom-made formulations produced by pharmacies when standard supply is limited or patients seek cheaper alternatives. Unlike FDA-approved GLP-1 drugs, compounded versions are not evaluated for safety, effectiveness, or quality, and their potency and purity can vary widely.
The FDA has warned that some compounded semaglutide products use salt forms that are not chemically or pharmacologically equivalent to approved drugs and that dosing errors with injectable compounded products have led to adverse events. Federal regulators have also issued warning letters to compounders marketing these alternatives as “generic” versions of FDA-approved medications. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/fdas-concerns-unapproved-glp-1-drugs-used-weight-loss
This list is not exhaustive, and individual risk assessment should always be done by a licensed clinician
Who should think twice before starting GLP-1 therapy
GLP-1s are powerful metabolic drugs and are not appropriate for everyone.
Extra caution is needed if you have:
- History of pancreatitis
- Gallbladder disease
- Severe gastrointestinal motility disorders
- Certain thyroid cancers (MEN2)
- Eating disorders
- Advanced kidney disease
- Recurrent dehydration
A rushed intake form cannot safely screen for these risks.
Who GLP-1 therapy tends to help most
While GLP-1 medications are not appropriate for everyone, they can be highly effective for the right patients when used responsibly.
GLP-1 therapy tends to benefit individuals who:
- Have a BMI ≥30, or BMI ≥27 with metabolic conditions such as prediabetes, hypertension, or dyslipidemia
- Have made repeated, sustained attempts at lifestyle change without durable weight loss
- Show signs of insulin resistance or metabolic syndrome
- Experience persistent “food noise” that interferes with healthy eating
- Are willing to view GLP-1s as a long-term medical tool, not a short-term fix
Importantly, the best outcomes are seen in patients who combine medication with nutrition education, resistance training, and ongoing monitoring, rather than relying on appetite suppression alone.
What proper monitoring should actually look like
A safe GLP-1 program should include baseline and follow-up monitoring, especially in the first 6–12 months.
At minimum, patients should discuss:
- Kidney function (creatinine, eGFR)
- Liver enzymes
- Blood glucose or HbA1c
- Electrolytes if nausea or vomiting occurs
- Weight, muscle mass, and hydration trends
Many telehealth platforms rely heavily on self-reported data. That may be convenient — but it shifts medical responsibility onto the patient.
To learn more about protecting your kidneys, read our detailed blog
What the latest science (2026) tells us
Beyond weight loss and glucose control, GLP-1 receptor agonists are increasingly recognized for their cardiovascular and metabolic benefits. Meta-analyses of large cardiovascular outcome trials show that drugs like semaglutide and other GLP-1 receptor agonists are associated with statistically significant reductions in major adverse cardiovascular events (MACE) such as heart attack and stroke, as well as improvements in blood pressure and lipid markers — indicating benefits that extend well beyond simple weight reduction. https://www.nejm.org/doi/full/10.1056/NEJMoa2307563
On the brain health front, emerging research suggests these medications may improve insulin signaling in the brain, reduce systemic and neural inflammation, and are associated with lower observed rates of dementia in large cohort studies, though definitive causal evidence from randomized trials is still pending. https://pmc.ncbi.nlm.nih.gov/articles/PMC12765848
Some early evidence also suggests improvements in appetite-related reward processing and mental well-being — sometimes described as a reduction in “food noise” — but more research is needed to confirm how these effects translate into clinical practice. https://www.news-medical.net/news/20250216/Diabetes-drugs-may-boost-brain-health-but-experts-warn-of-risks.aspx
Known risks — and the ones people rarely mention
Common side effects
- Nausea (≈40%)
- Vomiting, constipation, diarrhea
- Fatigue and dizziness
Less discussed but important
- Lean muscle loss during rapid weight reduction
- Bone density decline without resistance training
- Kidney stress from dehydration
- Gallbladder complications
“Most of these risks are manageable with proper dosing, hydration, nutrition, and follow-up.”
Protecting muscle and bone during GLP-1–driven weight loss
Rapid weight loss—especially when driven by appetite suppression—can lead to loss of lean muscle and bone density, not just fat.
This risk increases when:
- Protein intake drops unintentionally
- Resistance training is absent
- Weight loss exceeds the body’s ability to adapt
To reduce these risks, clinicians increasingly recommend:
- Adequate protein intake, often higher than traditional dieting norms
- Resistance or strength training 2–3 times per week
- Monitoring muscle mass trends, not just scale weight
The number on the scale alone does not reflect metabolic health. Preserving muscle is essential for long-term weight maintenance, glucose control, and physical independence—especially as people age.
Why GLP-1s can stress the kidneys and pancreas
GLP-1 drugs slow digestion and suppress appetite. When nausea or vomiting reduces fluid intake, dehydration can quietly develop.
Dehydration reduces kidney filtration, concentrates waste products, and increases the risk of acute kidney stress. Rapid changes in digestive signaling may also irritate the pancreas or gallbladder in susceptible individuals.
These risks are manageable — but only when recognized early and monitored properly.
The rebound reality: what happens when you stop?
GLP-1s suppress appetite — they do not permanently change biology.
When medication stops:
- Hunger signals return
- Metabolic rate may remain suppressed
A substantial portion of lost weight may return in many patients without structured maintenance support
Exit-strategy planning matters as much as starting therapy.
Clinical trials vs real life: the 50% gap
2026 research shows real-world patients often lose 40–50% less weight than clinical trial participants.
Trials include coaching, frequent follow-ups, and strict protocols. Real life often does not.
Medication works best when paired with:
- Nutrition education
- Behavior change support
- Resistance training
What’s next: beyond today’s GLP-1s
Retatrutide, a triple agonist targeting GLP-1, GIP, and glucagon receptors, has shown even greater fat loss in early trials.
But long-term safety data is still emerging. Progress must be balanced with caution.
Safe steps if you’re considering GLP-1 telehealth
- Verify pharmacies using NABP’s .pharmacy checker
https://safe.pharmacy - Start at the lowest effective dose
- Ensure kidney and metabolic monitoring
- Pair medication with nutrition and behavior coaching
- Avoid platforms promising “guaranteed” results
📄 Downloadable resource: GLP-1 Telehealth Safety Checklist (PDF)
Questions to ask any GLP-1 telehealth provider
- Is this FDA-approved or compounded?
- How will side effects be monitored?
- What labs are required and how often?
- What happens if I stop the medication?
- Who do I contact if symptoms worsen?
A warning about non-prescription GLP-1 products online
Many websites now sell “oral semaglutide drops,” “GLP-1 peptides,” or “no-prescription Ozempic alternatives.”
These products are not FDA-approved, often illegally marketed, and sometimes chemically unrelated to real GLP-1 drugs.
If a site claims no prescription is needed — that alone is a red flag.
To know more about AI in healthcare and what patients should know, check our detailed blog
Regulation, lawsuits, and rising scrutiny
The FDA has warned against unapproved GLP-1 compounds, and the FTC is investigating deceptive weight-loss marketing. Lawsuits have already emerged over billing practices and safety lapses.
Until oversight matures, patients must be informed advocates for their own health.
FAQs
It can be safe if you use legitimate providers requiring valid prescriptions. However, risky sites often skip necessary physical exams or labs. Always verify pharmacies using the NABP’s website and ensure the platform offers ongoing medical monitoring.
No. There is currently no FDA-approved generic semaglutide. Compounded versions are custom-made, not FDA-approved, and lack the rigorous safety data and standardized dosing of patent-protected drugs like Wegovy or Ozempic.
Likely, yes. GLP-1s suppress appetite but do not permanently change your biology. Without long-term maintenance or a structured transition plan involving nutrition and exercise, up to two-thirds of lost weight often returns.
No. Legitimate GLP-1 drugs always require a prescription. Websites selling “no-prescription” alternatives are often marketing unregulated or illegal products that may not contain real medication. This is a major safety red flag.
Nausea affects about 40% of patients, along with potential vomiting or constipation. Less discussed risks include the loss of lean muscle and bone density, making resistance training and protein intake essential during treatment.
Telehealth subscriptions often start around $79 monthly, but this usually covers just access or coaching. The medication cost is separate and can be significantly higher if your insurance denies coverage for weight-loss drugs.
Avoid these drugs if you have a history of pancreatitis, gallbladder disease, severe GI issues, or thyroid cancer (MEN2). A rushed online intake form may not catch these risks, so be transparent with your provider.
Final takeaway
GLP-1 drugs are powerful tools — not magic solutions.
Use them wisely. Monitor them carefully.
And never outsource your health to marketing promises.
👉 If this guide helped you, share it — and explore our other evidence-based articles to build a safer, smarter health journey.
